What is Degenerative Disc Disease?
Degenerative Disc Disease (DDD) refers to gradual, age-related deterioration of the intervertebral discs of the spine. In DDD, a detrimental cascade of changes in cellular, biochemical, structural and functional properties of spinal discs often results in back pain1. Although DDD may occur anywhere in the spine, it commonly affects the low back and the neck.
Degenerative Disc Disease is a misnomer; the condition is not actually a disease. In fact, gradual degeneration of the intervertebral discs is a natural part of the aging process. Although many people with disc degeneration experience pain, some individuals with DDD experience no symptoms.
In most people, the spine or vertebral column is comprised of 33 interlocking bones, or vertebrae, which are connected by fibrous bands called ligaments and divided into five regions:cervical, thoracic, lumbar, sacral and coccygeal. The vertebral column provides support for the upper body as well as protection for the spinal cord, and furnishes attachment points for the ribs and muscles of the back.
Another consequence of reduced intervertebral space is worsening instability of the spine. The body attempts to correct this instability with bony growths called bone spurs (osteophytes). Bone spurs can compress the spinal cord and nerve roots that extend from the spinal cord, resulting in pain. This instability can also cause painful muscular spasm in the low back as the body attempts to stabilize itself.
An additional problem caused by Degenerative Disc Disease is development of tears in the outer layer of the disc. This layer, known as the annulus fibrosis, is composed of tough, minimally innervated tissue. Significant pain may occur when a tear in the annulus fibrosis allows nerves on the periphery of the disc to grow further into the disc and become painful.
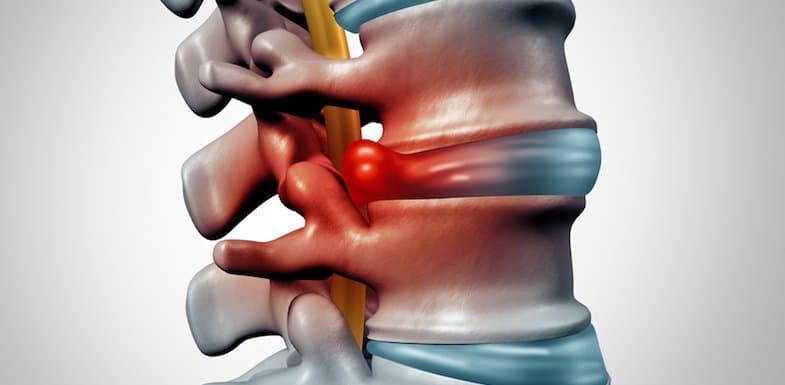
Pain also arises when excess pressure is put on a degenerating disc, which may cause the jelly-like substance within the disc to prolapse through tears in the annulus, resulting in a herniated disc. The disc itself may bulge out of place, producing local nerve irritation and compression of the spinal cord, a condition known as a bulging disc. Compression produced by herniated and bulging discs may cause local irritation of nerves and the spinal cord.
Pain may also arise when inflammatory proteins within prolapsed nucleus pulposus come into contact with a nerve root. This can cause extreme irritation and a painful inflammatory response in the nerve root. Termed radiculitis, this type of pain is frequently described as “shooting” since it travels from the spine outward. For example, pain from a compressed nerve may shoot down an arm or leg. When radiculitis goes untreated, complications such as muscle atrophy, reflex changes, and sensory loss may occur over time. In addition, a patient may begin to favor an unaffected side, causing overdevelopment of muscles on that side. This more severe nerve root condition is known as radiculopathy and underscores the importance of seeking help for radiating nerve pain.
Causes of Degenerative Disc Disease
Although development of Degenerative Disc Disease can simply be a natural consequence of aging and may be to some extent a hereditary condition2, there are certain measures an individual can take to help lower the likelihood of being diagnosed with DDD. Degenerative changes in DDD happen more often in people who smoke. They are also found more frequently in people who do heavy physical work, such as repetitive lifting. Individuals who are obese are also more likely to have symptoms of DDD. The validity of these risk factors is supported by a study of 344 people who had an MRI and completed low back pain questionnaires at the age of 40 and again at 44 years3. The authors of the study reported that disc-related MRI findings (e.g., disc degeneration, disc bulges, disc herniation) were concurrent with certain lifestyle factors (e.g., high physical work, high body mass index, and heavy smoking).
Yet another risk factor for DDD may be atherosclerosis, which can obstruct branching arteries of the abdominal aorta, including four paired lumbar arteries and the middle sacral artery that feed the lumbar spine. Researchers searched medical literature for studies involving atherosclerosis, DDD and low back pain, and discovered that post-mortem studies showed an association between atheromatous lesions in the aorta and DDD, as well as between occluded lumbar arteries and low back pain reported while the patients were alive4. In clinical studies, aortic calcification was associated with low back pain, and stenosis of lumbar arteries was associated with both DDD and low back pain. In epidemiological studies, smoking and high serum cholesterol levels were found to have the most consistent associations with DD and LBP. The collective findings of these studies support the importance of maintaining good cardiovascular health to thwart DDD. Heart-healthy habits include consuming a diet low in fat and sodium, getting regular exercise, avoiding smoking, and lowering stress.
Diagnosing Degenerative Disc Disease
A doctor may order a variety of tests to help determine whether a person’s pain is caused by Degenerative Disc Disease. Some of these tests may include:
- Imaging studies – MRI, CT scan and X-ray are used to help practitioners visualize structures that may be causing pain.
- Medial Branch Blocks (MBBs) – Medial Branch Blocks are a minimally invasive non-surgical treatment used for neck and back pain. Diagnostically, MBBs are used to test whether pain-producing medial branch nerves will respond to more permanent interruption by a radio-frequency ablation. They also have a therapeutic effect in that they reduce inflammation and irritation in the facet joints of the spine.
- Selective Nerve Blocks – These are used to help the practitioner identify which nerves are causing pain. By selectively numbing each nerve, pain-causing nerves can be identified and treated.
- Discography – Discography involves the use of contrast dyes to obtain a detailed image of intervertebral discs. It is used to evaluate patients whose back pain has not improved with comprehensive conservative care regimens. It provides the doctor with detailed information on the pain potential of the affected area, and is commonly used for surgical planning prior to a lumbar fusion.
Degenerative Disc Disease Treatment
Since Degenerative Disc Disease is an irreversible process, treatment focuses on managing symptoms. Treatment of back pain depends upon the nature and severity of the pain. In general, minimally invasive procedures are tried before more aggressive procedures are used. Aggressive procedures are reserved as a last resort as they are associated with higher risks.
An abundance of research supports the efficacy of non-surgical procedures in treating pain that arises from DDD. Below is a basic overview of diagnostic procedures and pain relief options:
- Pharmacotherapy – Administration of non-steroidal anti-inflammatory drugs (NSAIDs, or Ibuprofen-like drugs), acetaminophen (Tylenol), muscle relaxants, and membrane stabilizing medications is often effective in treating low back pain. Our doctors are highly trained in pain medication management.
- Physical Therapy – Physical therapies aim to promote healing in the disc periphery, by stimulating cells, boosting metabolite transport, and preventing adhesions and re-injury. Such an approach may have the potential to accelerate pain relief in the disc periphery, even if it fails to reverse age-related degenerative changes in the nucleus5.
- Epidural Steroid Injections (ESIs) – Frequently, epidural injections are used for degenerative disc disease and other pain syndromes. The doctor injects a steroid into the epidural space of the spinal cord, where the irritated nerve roots are located. The medicine then spreads to other levels and portions of the spine, reducing inflammation and irritation. A study in patients with chronic lumbar discogenic pain found ESIs with or without steroids lowered pain 80% of patients tested6.
- Facet injections – Facet injections, a minimally invasive procedure, lower painful inflammation and irritation in the facet joints of the spine. The injected medication includes a combination of local anesthetic and long-lasting steroid. By numbing affected nerves, the injection temporarily halts transmission of pain signals to the brain, and the slow-release steroid combats inflammation. The efficacy of facet joint injections is supported by a recent study in patients with large lumbar disc herniation who were treated with facet injections. The overall efficacy was 91.4% and the researchers concluded facet injection via the posterior-lateral route and inner margin of the facet joint is effective and safe for treatment of large lumbar disc herniation7.
- Spinal Cord Stimulation (SCS) – An implanted electrical device decreases the perception of pain by confusing the spinal cord and pain processing centers of the brain. Initially a trial is conducted to determine whether this device will help the patient on a long-term basis. It is effective in about 50–70% of patients8.
- Lysis of Adhesions (Racz Procedure) – This procedure helps remove excessive scar tissue in the epidural space. It is used in vertebral body compression fractures, post-laminectomy syndrome, radiculopathy, and DDD.
- Peripheral Nerve Stimulation – This method involves placement of tiny electrodes near the affected nerves. The electrodes release a small electrical current that inhibits pain transmission and provides pain relief.
- Percutaneous Discectomy – A needle is inserted through the skin into the affected disc, material is suctioned out of the bulging disc and pressure is relieved within the disc.
- Cryotherapy – Affected nerves are identified via electrical stimulation and destroyed by freezing cycles.
Radiofrequency Ablation – Nerves branching away from the spinal cord (peripheral nerves) can be blocked with local anesthetic, after which nerve ablation or destruction can be initiated. - Trigger Point Injections – These injections can extremely successful in alleviating musculoskeletal pain. A local anesthetic and steroid are injected into a “trigger point.”
- Biofeedback – This therapy teaches awareness of processes normally thought to be involuntary inside of the body such as blood pressure, temperature and heart rate, enabling some degree of conscious control of these processes. Biofeedback can influence and improve level of pain and promotes relaxation.
- Massage – Gentle focal rubbing of tender areas may help relieve muscle spasms or contractions and improve the discomfort associated with these events. Massage may also promote relaxation, decreasing stress and tension.
- Chiropractic Manipulations – Targeted physical “adjustments” may significantly reduce back pain, especially when combined with other modalities. Specialized manipulations intended to correct nerve transmission are delivered by a knowledgeable, experienced practitioner.
- Prolotherapy – Also known as Regenerative Injection Therapy, this technique involves injection of irritating substances into painful ligaments and tendons. The procedure is used to initiate the body’s natural healing processes.
- Surgery – Surgical procedures are a last resort when conservative treatments are unsuccessful in reducing pain or when the spinal cord or exiting nerves are being severely compressed. Serious compressions may be characterized by bladder and bowel incontinence, lower extremity weakness, spasticity, and loss of sensation. Invasive surgical procedures include discectomy, laminectomy, spinal fusion and spinal instrumentation. Since surgery carries the risk of complications, it is used only when less invasive procedures have failed to restore functionality and provide relief.
When pain from Degenerative Disc Disease threatens to diminish quality of life, consult with the knowledgeable practitioners at Wake Spine & Pain Specialists. The caring doctors at our pain clinic have received extensive training in foremost pain management techniques and development of optimized, tailored pain management regimens.
References
- Smith, LJ, Nerurkar, NL, Choi, KS, Harfe, BD, & Elliott, DM. (2011). Degeneration and regeneration of the intervertebral disc: lessons from development. Dis Model Mech., 4(1), 31-41.
- Videman T, Battié MC, Parent E, Gibbons LE, Vainio P, & Kaprio J. (2008). Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine (Phila Pa 1976)., 33(13), 1484-90.
- Jensen TS, Kjaer P, Korsholm L, Bendix T, Sorensen JS, Manniche C, & Leboeuf-Yde C. (2010). Predictors of new vertebral endplate signal (Modic) changes in the general population. Eur Spine J., 19(1):129-35.
- Kauppila LI.(2009). Atherosclerosis and disc degeneration/low-back pain–a systematic review. Eur J Vasc Endovasc Surg., 37(6), 661-70.
- Adams MA, Stefanakis M, & Dolan P. (2010). Healing of a painful intervertebral disc should not be confused with reversing disc degeneration: implications for physical therapies for discogenic back pain. Clin Biomech (Bristol, Avon)., 25(10), 961-71.
- Manchikanti L, Cash KA, McManus CD, Pampati V, & Benyamin RM. (2010). Preliminary results of a randomized, double-blind, controlled trial of fluoroscopic lumbar interlaminar epidural injections in managing chronic lumbar discogenic pain without disc herniation or radiculitis.
Pain Physician., 13(4), E279-92. - Lu W, Li YH, & He XF.(2010). Treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral route and inner margin of the facet joint. World J Radiol., 2(3), 109-12.
- Kunnumpurath S. (2009). Spinal cord stimulation: Principles of past, present and future practice: A review. Journal of Clinical Monitoring and Computing, 23, 333-339.


