What is Sciatica?
Sciatica refers to pain that may be caused by compression and irritation of the sciatic nerve, or of any of the five spinal nerve roots that give rise to each sciatic nerve. There are two sciatic nerves. They travel from the low back through the buttock and down the back of the leg and foot. In addition to pain along the length of the sciatic nerve, other symptoms of sciatica may include numbness, muscle weakness, tingling, and difficulty with movement. Symptoms are usually unilateral, meaning they occur in only one sciatic nerve at a time, although sometimes symptoms are perceived on both sides.
The pathophysiology of sciatica is not completely understood, although the current understanding is that mechanical alterations combined with inflammatory changes lead to pain. Compression may alter nerve root conduction and deprive spinal nerve roots of nutrition, mechanical forces may lead to nerve damage and functional changes in nerve roots, and chemical and metabolic effects may create an inflammatory response (Garfin et al, 1995). Varying causes of inflammation coupled with varying degrees of compression can occur anywhere along the cauda equina, or the bundle of nerve roots at the lower end of the spinal column, and contribute to the pain response and neurologic deficits associated with sciatica.
It is important to note that sciatica is not a disease, but a term used to describe an array of symptoms including pain. This point is important, because treatment for the symptoms will depend upon the underlying cause.
The friendly doctors at Wake Spine & Pain Specialists have years of experience in the treatment of sciatica. We understand the stress and inconvenience of living with a painful condition and encourage you to seek help as soon as possible to prevent your condition from worsening.
Causes of Sciatica
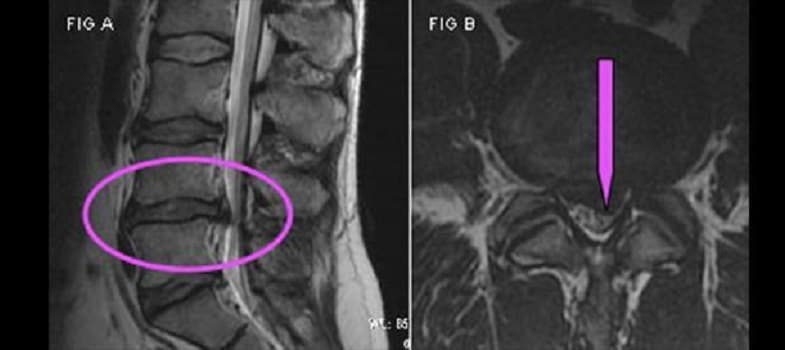
Another cause of sciatica is spinal stenosis, or progressive narrowing of the spinal canal causing spinal nerve or spinal cord compression. This narrowing can be caused by bone spurs, spondylolisthesis, inflammation, and herniated discs, which decrease available space for the spinal cord. This narrowing also pinches and irritates lumbar and sacral spinal nerves, which in turn affect sciatic nerves. Spinal stenosis often results in persistent pain in the low back and lower extremities, which may include sciatica. Difficulty walking, decreased sensation in the lower extremities, and decreased physical activity are other symptoms of the disorder. Many people with spinal stenosis present with bilateral sciatica, meaning both sciatic nerves are affected.
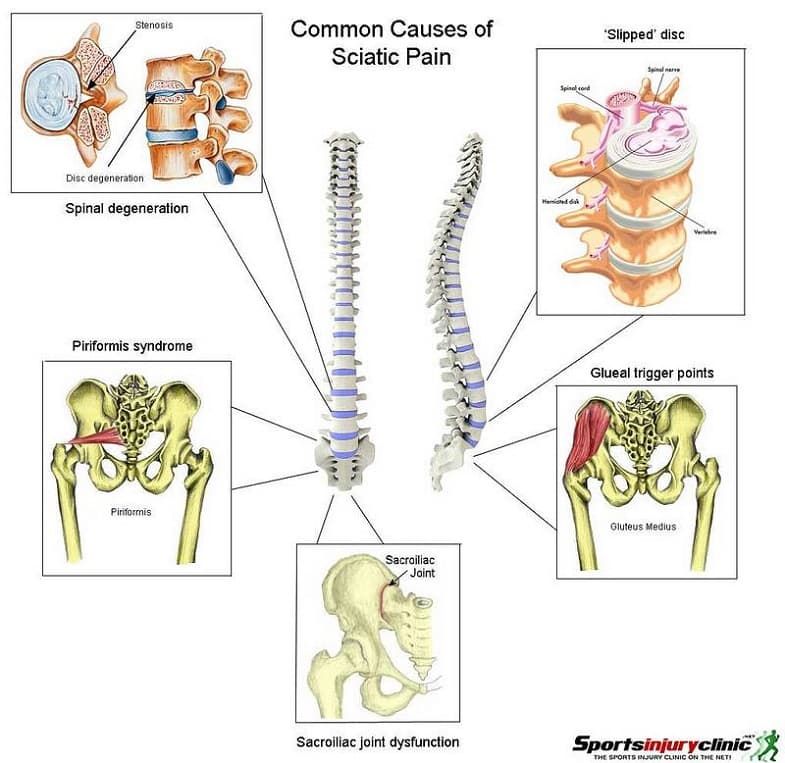
Piriformis syndrome may also be responsible for the development of sciatica. The piriformis is a large pelvic muscle. In some people, the sciatic nerve runs through the piriformis muscle rather than beneath it. When the muscle spasms due to trauma or overuse, it can compress the sciatic nerve beneath the muscle. Conditions of this type are generally referred to as entrapment neuropathies; in the case of sciatica and the piriformis muscle, the entrapment neuropathy is known as piriformis syndrome. Colloquially, the condition has been called “wallet sciatica” since a wallet carried in a rear hip pocket compresses the muscles of the buttocks and sciatic nerve when the bearer sits. Although routine treatment for PS has focused on physical therapy, and possibly injections of pain-relieving and steroid medications, recently the use of botulinum toxin (botox) has gained popularity (Kirschner et al, 2009). Its use is aimed at relieving sciatic nerve compression and inherent muscle pain from a tight piriformis.
Sciatica may also be experienced in pregnancy, primarily due to the enlarged uterus pressing on the sciatic nerve. It is also caused by the muscular tension, vertebral compression, and postural changes caused by carrying extra weight. Sciatica associated with pregnancy may or may not resolve after the baby is born.
Treatment for Sciatica
Initially, treatment of sciatica focuses on lowering the inflammation that is causing symptoms. This may include taking non-steroidal anti-inflammatory drugs (NSAIDs) and muscle relaxers, and resting. In some cases, your doctor may prescribe oral steroids, which have more severe side effects but are proven effective in treating more stubborn cases of inflammation.
Patient Review, Lower Leg Pain Gone!
When the initial pain of sciatica subsides, exercises and physical therapy may be a beneficial part of your treatment program. Application of heat and cold may soothe the affected area.. Sometimes, your doctor may administer an epidural steroid injection (ESI) containing anti-inflammatory medication directly into to the inflamed area.
As with other conditions, surgery in sciatica patients is used only as a last resort. More conservative treatment modalities are tried first, since surgery carries a higher risk of complications. If surgery is performed, the goal may be to create more room for a nerve that is being compressed. To achieve this, your doctor may need to remove a deteriorated spinal disc, extract tissues around the nerve, or perform a different surgical intervention.
A list of the different treatment modalities for sciatica includes:
- Pharmacotherapy – The treatment of sciatica may include medications like NSAIDs (Ibuprofen-like drugs), acetaminophen, membrane stabilizing drugs, muscle relaxants, and other analgesics.
- Epidural Steroid Injections (ESI) – These injections deliver a long-lasting steroid and a local anesthetic into the epidural space, targeting the irritated nerve root. The steroid reduces inflammation and irritation and the anesthetic works to interrupt the pain-spasm cycle and transmission of pain signals (Boswell et al, 2007). The combined medicines then spread to other levels and portions of the spine, reducing inflammation and irritation. The entire procedure usually lasts under fifteen minutes. ESIs have been shown to provide rapid relief of symptoms that allows patients to regain normal daily activity (Vad V et al, 2002). A large study in 2005 including two hundred and twenty-eight patients with a clinical diagnosis of unilateral sciatica were randomized to either three lumbar ESIs of or a placebo injection at intervals of three weeks. The ESI group demonstrated a 75% pain improvement over the placebo group (Arden et al, 2005).
- Lysis of Adhesions – This procedure, also known as the “Racz Procedure“ has been shown to be effective in removing excessive scar tissue in the epidural space (Racz et al, 2008). Since it is more invasive than other treatments, more conservative measures are typically tried before resorting to this procedure.
- Infusions Techniques – The procedure involves extended delivery of local anesthetic and other medications through a small catheter that is inserted through a needle into the epidural space or in the region of affected nerves. When pain from the nerves is blocked continuously with an infusion, pain relief can be dramatic and long lasting. A Finnish study showed a beneficial effect of a single infusion of 3 mg/kg of infliximab for herniation-induced sciatica, which was sustained in most patients over a 1-year follow-up period (Korhonen T et al, 2004).
- Transcutaneous Electrical Stimulation (TENs) – This passive process decreases the perception of acute and chronic pain and is not associated with side effects. Mild electrical current is delivered topically via patches placed on the skin over the affected area. Delivery of electrical stimuli confuses the spinal cord and brain pain processing centers, and painful signals are replaced by tingling electrical signals. This promotes relaxation of the muscle, improves mobility, and pain relief.
- Spinal Cord Stimulation (SCS) – In this treatment modality, your doctor implants an electrical device that decreases the perception of pain by confusing the spinal cord and brain pain processing centers. Initially a trial is done to see if this device will be of benefit to you long-term. In the initial trial, your pain physician places a small electrical lead through a needle in the epidural space. Painful signals are replaced by tingling electrical signals. If you experience significant pain relief in your trial, you may opt to have a permanent SCS device implanted.
- Deep Tissue Massage – Focal rubbing of tender areas may help relieve muscle spasms or contractions and improve the discomfort associated with sciatica. Massage can also promote relaxation, decreasing stress and tension.
- Physical therapy – Physical Therapy helps improve symptoms of sciatica by increasing flexibility, range of motion, posture, and improving muscle strength. In fact, current evidence shows that an active exercise program promotes early recovery in sciatica patients (Goh L et al, 2003).
- Nutrition and Exercise – Exercise improves the pain of sciatica by increasing flexibility and range of motion. Another benefit is the releases hormones called “endorphins,“ which are your body’s natural pain relievers. Nutrition and healthy eating may be powerful treatments to combat nutritional deficits.
- Intrathecal Pump Implants – In some patients, implanted pain pumps can provide significant long-term pain control. The effectiveness of intrathecal therapy in patients suffering from nociceptive pain showed a pain reduction in 66.7% of patients experiencing pain due to cancer (Becker 2000).
- Disc Decompression – This technique is used to treat a bulging disc. A needle is inserted into the affected disc through the skin, and disc material is aspirated. The primary goal of the procedure is to relieve pressure within the disc.
- Trigger Point Injections (TPIs) – These are used to calm muscle spasms. A local anesthetic and steroid into a trigger point, or an affected area where the muscle has become ischemic (or starved of nutrients), which is painful. Performing a piriformis muscle injection is considered a type of TPI.
- Botox (Botulinum Toxin) – Advocates of Botox suggest its properties can reduce muscle spasms, ischemia and inflammatory markers, thereby reducing pain. In a review of three studies that investigated the merits of botox for low back pain, one trial found that botox injections were better than injections of corticosteroid plus lidocaine or placebo in patients with sciatica attributed to piriformis syndrome (Waseem Z et al, 2011).
- Biofeedback – Biofeedback is a treatment that teaches a patient to become aware of processes that are normally thought to be involuntary inside of the body (such as blood pressure, temperature and heart rate control). The goal is to gain some degree of conscious control over these processes, which can influence and improve your level of pain. Improved self-awareness may help a person to relax effectively and this can promote pain relief.
- Spinal manipulation (Chiropractic treatment) – Some sciatica patients may derive benefit from spinal manipulation. A study comparing the clinical efficacy of spinal manipulation against microdiskectomy in patients with sciatica secondary to lumbar disk herniation found 60% of patients with sciatica who had failed other medical management benefited from spinal manipulation to the same degree as if they underwent surgical intervention (McMoreland G et al, 2010).
Wake Spine & Pain Specialists cares about your quality of life and understands the burden of living with pain. Our caring practitioners will work with you to design a customized treatment plan that restores your health as quickly, efficiently and non-invasively as possible. With our numerous combined years of experience, we are confident we can design the best pain management plan for you. Call our pain clinic today to schedule an appointment.
Sources
- Arden NK et al. (2005). A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: the WEST study. Rheumatology (Oxford).;44(11):1399-406.
- Boswell M et al. (2007). Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 10(1):7-111.
- Garfin et al. (1995). Spinal nerve root compression. Spine (Phila Pa 1976). 20(16):1810-20.
- Goh L et al. (2003). An evidence-based approach to the management of low back pain and sciatica: how the evidence is applied in clinical cases. Musculoskeletal Care. 2003 Sep;1(2):119-30.
- Kirschner et al. (2009). Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 40(1):10-8.
- Korhonen T et al. (2004). Efficacy of infliximab for disc herniation-induced sciatica: one-year follow-up. Spine (Phila Pa 1976). 29(19):2115-9.
- McMorland G et al. (2010). Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. J Manipulative Physiol Ther. 33(8):576-84.
- Racz GB et al. (2008). Percutaneous lysis of epidural adhesions–evidence for safety and efficacy. Pain Pract. 8(4):277-86.
- Vad VB et al. (2002). Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976). 1;27(1):11-6.
- Waseem Z et al. (2011). Botulinum toxin injections for low-back pain and sciatica. Cochrane Database Syst Rev. (1):CD008257.