What Is Radiofrequency Ablation?
Radiofrequency ablation is a treatment method that involves the use of radio waves to produce heat that targets damaged nerves in order to relieve chronic pain. The heat is in the form of an electrical current and it disrupts pain signal transmission from the affected nerves on a semi-permanent basis by completely destroying or temporarily impairing nerve tissue.
This procedure was initially introduced during the 1930s as a treatment for trigeminal neuralgia, a condition that is characterized by sharp, intense facial pain. Radiofrequency ablation was first performed specifically to target the trigeminal nerve, the source of the facial pain, and the procedure was successful. Currently, facet joint pain, especially in the lumbar region (lower back), is commonly treated with radiofrequency ablation. Facet joints are bony structures that connect spinal vertebrae to one another. If the nerves that extend out of the facet joints become damaged, chronic pain can develop. Radiofrequency ablation is often performed to destroy the affected nerves and stop the transmission of pain signals. This procedure has also been effectively utilized for lumbar back pain, neck pain, and arthritic pain.
Research has shown that the interruption of nerve function through the application of electrical currents results in long-term pain relief that lasts longer than when other conventional treatments are used. Most patients who undergo radiofrequency ablation report dramatic relief that persists for six months up to one year. There are two forms of radiofrequency ablation called pulsed and continuous radiofrequency and both forms successfully inhibit pain signal transmission from damaged nerves, thereby reducing pain.
How Is Radiofrequency Ablation Performed?
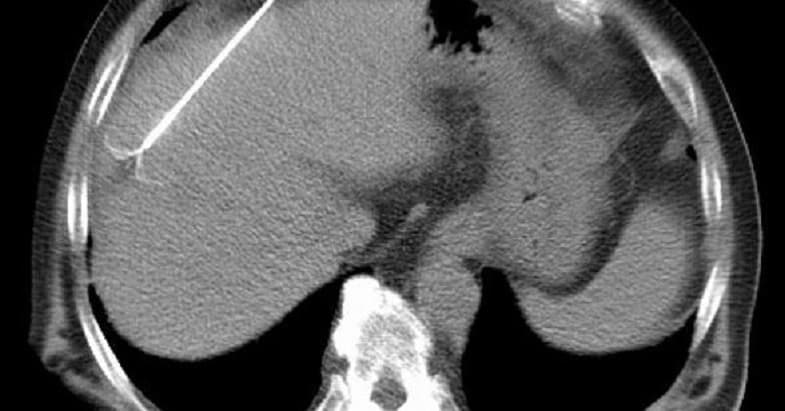
Before the radiofrequency ablation procedure is performed, an anesthetic is usually intravenously (IV) administered to the patient to reduce discomfort. Next, a physician will use imaging technology (e.g., fluoroscopy) to guide the placement of a special needle into the region of the spinal column where the affected nerves are located. After the correct position has been confirmed, a microelectrode that will provide the electrical current-induced heat is fed through the needle.
A mild electrical current is applied during the insertion of the microelectrode. This causes the patient to feel a tingling sensation and allows the physician to observe the patient’s motor and sensory responses to the stimulation. Nerves that are responsible for motor functions should not be directly targeted even if they are responsible for the pain as damage to such nerves may cause motor deficits.
After the optimal placement of the needle and electrode are confirmed, the physician will then initiate the continuous frequency or the pulsed frequency. Continuous radiofrequency ablation involves gradually increasing the frequency of the current until the electrode produces a temperature of 122-176°F (50-80°C). Once the appropriate temperature is reached, it is maintained for up to 90 seconds as this is the amount of time that is needed for the heat to disrupt nerve function.
Pulsed radiofrequency is similar to continuous radiofrequency, but the affected nerves are only exposed to short pulses of current for approximately 20 milliseconds followed by a cool-down period of 480 milliseconds where no current is applied to the nerves. The temperature of the electrode only reaches between 104-107.8°F (40-42°C). The pulsed method produces a less severe amount of tissue damaged and is associated with fewer side effects.
In addition to the application of heat, sometimes steroids are also injected into the affected region to decrease inflammation that may have already been present or might develop temporarily after the procedure. While the procedure is being performed, the patient should not feel any pain due to the anesthetic that is administered.
If the patient’s level of relief is only minimal after undergoing radiofrequency ablation treatment, then it can be repeated two or three weeks later. Usually the nerves that were targeted during the treatment tend to regrow by six to 18 months, but the degree of pain that was experienced before the procedure usually does not return, although mild pain may be felt. In addition, individuals who begin physical therapy after treatment and remain physically active often maintain low pain levels and tend to benefit from increased muscle strength. Nonetheless, if a significant degree of pain returns, another ablation treatment can be safely performed.
There are a few risks that are associated with radiofrequency ablation treatment, such as the occurrence of an infection or permanent nerve damage. The needle and the microelectrode are placed close to the affected nerves and, in some cases, this causes pain to slightly increase. Pain may also be felt in the extremities, but if this does occur it is generally temporary. In addition, there is the risk that motor nerves and blood vessels that are near the damaged nerves may become injured. Moreover, the electrical current that produces heat during the treatment can potentially cause electrical burns, but the occurrence is rare.
Conditions Associated With Radiofrequency Ablation
Early research that demonstrated the beneficial effects of radiofrequency ablation mainly focused on facet joint pain in the lower back (lumbar region). Clinical studies also showed that this technique could be used to decrease the size of bone spurs and tumors. As its application was expanded for additional conditions, it demonstrated effectiveness for a wide variety of health problems.
Conditions that have been successfully treated with radiofrequency ablation include:
- Lumbar facet joint pain
- Neck pain (cervical facet pain)
- Arthritic pain
- Herniated intervertebral disc (dorsal root ganglion)
- Trigeminal neuralgia (trigeminal ganglion)
- Sympathetic ganglia
- Atypical facial pain and chronic headaches (sphenopalatine ganglion)
- Sacroiliac joint complex (low back pain)
Patient Review of Radiofrequency Ablation
Conclusion
Radiofrequency ablation is used to treat chronic pain through the use of radio waves that produce electrical current-induced heat. The heat is applied to damaged nerves that have been causing pain and this process leads to the disruption of pain signal transmission.
This procedure is minimally invasive and has been shown to be effective for a number of different conditions. The heat can be applied in a continuous or pulsed manner and both approaches cause the semi-permanent inhibition of nerve function. Patients generally report dramatic pain relief after this procedure has been performed.
References
- Bayer E, Racz GB, Miles D, Heavner J. Sphenopalatine ganglion pulsed radiofrequency treatment in 30 patients suffering from chronic face and head pain. Pain Pract. 2005; 5(3): 223-227.
- Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007; 10(1): 229-253.
- Burnham RS, Yasui Y. An alternate method of radiofrequency neurotomy of the sacroiliac joint: a pilot study of the effect on pain, function, and satisfaction. Reg Anesth Pain Med. 2007; 32(1): 12-19.
- Byrd, D., MacKey, S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008; 12(1): 37-41.
- Chao, S, Lee, H, Kao, T, Yang, M, Tsuiei, Y, Shen, C, Tsou, H. Percutaneous pulsed radiofrequency in the treatment of cervical and lumbar radicular pain. Surg Neurol. 2008; 70: 59-65.
- Cohen, SP, Sireci, A, Wu CL, Larkin, TM, Williams, KA, Hurley, RW. Pulsed radiofrequency of the dorsal root ganglia is superior to pharmacotherapy or pulsed radiofrequency of the intercostal nerves I the treatment of chronic postsurgical thoracic pain. Pain Physician. 2006; 9: 227-235.
- Knoll, HR, Kim, D, Danic, MJ, Sankey, SS, Gariwala, M, Brown, M. A randomized, double-blind, prospective study comparing the efficacy of continuous versus pulsed radiofrequency I the treatment of lumbar facet syndrome. J of Clin Anesth. 2008; 20: 534-537.


