What is a Herniated Disc?
It is estimated that 84% of adults will suffer from some type of lower back pain; in fact, lumbar back pain is such a common ailment that it accounts for approximately 2.3% of all doctor visits2, 3. Most back pain cases resolve on their own in a few weeks with conservative treatment, but some cases persist beyond six weeks. These cases are often due to a condition termed a ‘herniated disc,’ which accounts for 2% of all back pain cases8.
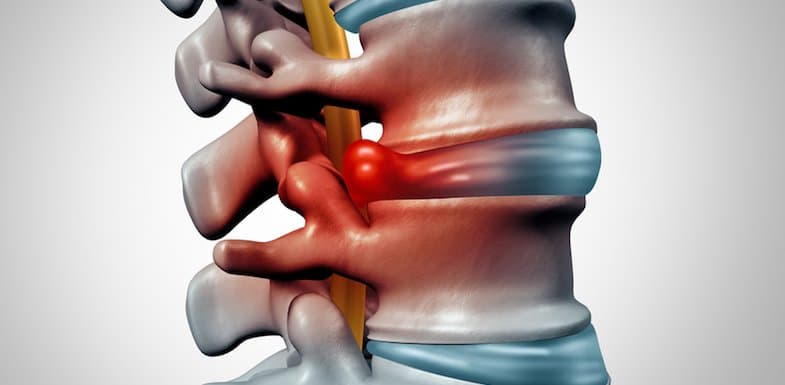
A herniated disc is generally described as movement of an intervertebral disc outside of its normal space, or joint1. Intervertebral discs separate and cushion the individual bones, or vertebrae, that comprise the spine5. These cartilaginous discs consist of a soft, gelatinous center, or nucleus pulposus, contained within a thick, fibrous capsule, or annulus fibrosus, which supports the weight of the upper body and create joints – giving the spine flexibility and allowing back movement6.
A herniated disc occurs when the nucleus pulposus pushes out through a weakening or tear in the annulus fibrosus7. Herniations of the lumbar (lower back) discs tend to be the most common, followed by herniations of the cervical (neck) discs4. Thoracic herniations are rare.
Patients with a herniation typically present with pain from compression of nearby nerve roots, termed radiculopathy. Progressive compression can lead to weakness in associated muscle groups and/or numbness in associated areas of skin. Patients with a cervical disc herniation present with spine tenderness on the neck and severe persistent pain in the neck and upper extremities, and patients with a lumbar disc herniation present with lower back pain which radiates down the back of the leg past the knee in 95% of patients11.
Diagnosing a Herniated Disc
Diagnosis of a disk herniation can be made by a doctor through a comprehensive history, physical exam, and neurological exam with supplemental imaging. A definitive diagnosis requires both symptoms consistent with herniation and visualization of the herniation by imaging; diagnostic imaging, however, is usually reserved for when pain is unresponsive to conservative treatment and persists beyond 4-6 weeks7.
Magnetic resonance imaging (MRI) is the gold standard for imaging disc herniation, and can visualize displacement of the nucleus pulposus as well as determine the extent of disc degeneration throughout the spinal cord10. Other diagnostic techniques include9:
- Computed tomography (CT) can be used when MRI isn’t available or possible
- X-Ray imaging can be used to rule out other possible causes before an MRI is performed
- Discography uses CT/MRI to image discs after contrast has been injected, and can be used for better visualization
- Nerve conduction tests can be done when isolating affected nerve roots is difficult
Patients and doctors alike should always be on the lookout for certain alarm symptoms if a herniated disc is suspected. Damaged lumbar discs can compress a certain group of nerve roots called the Cauda Equina, leading to impotence, incontinence (urinary or bowel) and numbness under the groin. This condition requires immediate surgical intervention to prevent long-term damage2.

Herniated Disc Treatment Options
Patients diagnosed with a herniated disc have a variety of treatment modalities available depending upon symptom severity and patient preference. Treatment typically begins with conservative pain management but can also include surgical and alternative approaches as necessary and/or desired. The best method for treating a herniation is to prevent it from occurring in the first place; prevention tips include12:
- Weight management through proper diet
- Maintaining strong, flexible muscles; walking or swimming are good choices
- Practice good posture and proper lifting techniques (using legs, not the back)
- A back brace may be useful periodically for spinal support
Mild cases of disc herniation may be treated conservatively.
- Physical therapy is the backbone of conservative pain management for herniated discs, and can include spinal manipulation, hot/cold therapy, ultrasound therapy, brace support and traction13.
- Over the counter non-steroidal anti-inflammatory medications (NSAIDS) such as aspirin, ibuprofen (Advil™) or naproxen (Aleve™) can be used for management of mild pain12.
- For the short term management of more severe pain, narcotic medications such as codeine or oxycodone can be prescribed12. Medications specific to controlling nerve pain, such as Gabapentin may be useful as well with lower risk than narcotics.
- Epidural steroid injections have been shown to directly reduce inflammation associated with disc herniation (and thus nerve root compression) yielding some benefit for pain14.
For symptoms that are more severe — or persist for many weeks — surgical intervention may be necessary. Open discectomy is the most common, and currently the gold standard, for treating herniations7. In this procedure part of the damaged disc is removed to alleviate pain and pressure. More minimally invasive procedures, such as the micro discectomy, have spawned from the open discectomy. Fusion of adjacent vertebral bones is also sometimes recommended to prevent recurrence of herniations4.
Alternative treatments for lower back pain show some benefit, most notably acupuncture. One recent study has shown acupuncture to be more effective than placebo13. The experts at Wake Spine & Pain Specialists can assist patients in determining the best course of action for dealing with back pain due to herniation of a disc.
Mild or moderate cases of disc herniation generally respond well to conservative therapy, while those cases that don’t will often respond well to surgical intervention15. Some 95% of patients can expect a positive outcome with appropriate pain management.
Spine surgery is a very active field in terms of improving the way in which surgeries are performed7. Discectomies, which have for years been open and invasive, are now often being performed through smaller incisions (arthroscopically) with reduced anesthesia. Artificial disc replacement surgery is also under investigation, however much research remains to be done to determine clinical effectiveness.
References
- Fardon, D.; Milette, P. Nomenclature and Classification of Lumbar Disc Pathology: Recommendations of the Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine, 2001. 26: p. E93-113.
- Wheeler, S.; et al. Approach to the diagnosis and evaluation of low back pain in adults. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2010.
- Deyo, R.A., S.K. Mirza, and B.I. Martin, Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976), 2006. 31(23): p. 2724-7.
- Rihn, J.; et al. Herniated intervertebral disc. First Consult, MD Consult Web site. Available at: www.mdconsult.com.ezproxy2.library.arizona.edu. Posted July 29, 2010. Accessed April 10, 2011.
- Hsu, P.; et al. Lumbosacral radiculopathy: Pathophysiology, clinical features and diagnosis. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2011.
- Raj, P. Intervertebral Disc: Anatomy-Physiology-Pathophysiology-Treatment. Pain Practice, 2008. 8: p. 18-44.
- North American Spine Society 2009: Lumbar (open) Microscopic Discectomy. Patient Handouts page. Available atwww.knowyourback.org/Pages/Treatments/SurgicalOptions/LumbarDiscectomy. Accessed April 15, 2011.
- Deyo, R.A., J. Rainville, and D.L. Kent, What can the history and physical examination tell us about low back pain? JAMA, 1992. 268(6): p. 760-5.
- Milette, P. Classification, diagnostic imaging, and imaging characterization of a lumbar herniated disc. Radiologic Clinics of North America, 2000. 36.
- Deen, H.G., Jr., Diagnosis and management of lumbar disk disease. Mayo Clin Proc, 1996. 71(3): p. 283-7.
- Marx, J.A., et al., Rosen’s emergency medicine : concepts and clinical practice. 7th ed. 2010, Philadelphia: Mosby/Elsevier. 2 v. (xxxvii, 2604, cviii p.).
- Clinical Reference Systems 2010: Herniated Disk. Patient Handouts page. MD Consult Web site, Core Collection. Available at www.mdconsult.com.ezproxy2.library.arizona.edu. Accessed April 15, 2011.
- Chou, R. and L.H. Huffman, Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med, 2007. 147(7): p. 492-504.
- Legrand, E., et al., Sciatica from disk herniation: Medical treatment or surgery? Joint Bone Spine, 2007. 74(6): p. 530-5.
- Nozawa, S., et al., Spontaneous disappearance of lumbar disk herniation within 3 months. Orthopedics, 2009. 32(11): p. 852.